Urgent Health Alert: The Hidden Dangers in Your Medicine Cabinet – What You NEED to Know About Blood Clots…
Imagine taking a pill every day, trusting it to help you, only to discover it could be putting your life at risk. It’s a terrifying thought, but it’s a reality we need to confront. Recently, health authorities worldwide have issued urgent warnings and even withdrawn certain medications due to a serious, silent threat: blood clots.
This isn’t about fear-mongering; it’s about empowering you with vital information. Your awareness could save your life, or the life of someone you love.
The Silent Threat: What Are Blood Clots (Thrombi) and Why Are They So Dangerous?
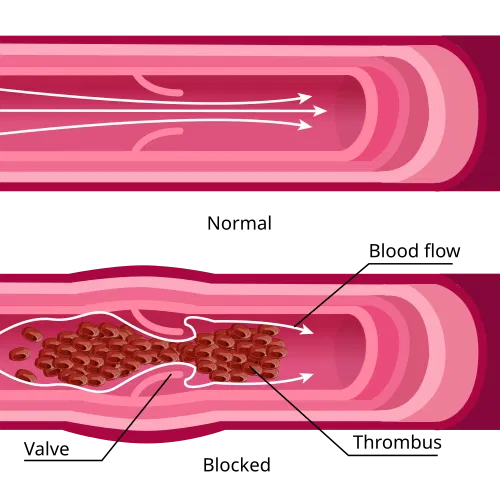
Think of your blood as a river. Normally, it flows smoothly, delivering oxygen and nutrients everywhere they’re needed. A blood clot (or thrombus) is like a dam forming in that river. While clotting is essential to stop bleeding when you get a cut, a clot forming inside your veins or arteries is a medical emergency.
These abnormal clots can:
Block blood flow to vital organs.
Lead to life-threatening conditions like:
- Pulmonary Embolism (PE): A clot in the lungs.
- Stroke: A clot blocking blood flow to the brain.
- Heart Attack: A clot in the arteries supplying your heart.
- Deep Vein Thrombosis (DVT): A clot, usually in the leg, that can break off and travel to the lungs.
Even a small clot can be fatal if it cuts off oxygen to a critical area. That’s why medications linked to increased clotting risks are taken extremely seriously by health agencies.

Is Your Medication on the Radar? What Pills Are Under Investigation?
While specific drug names can vary by country and regulatory decisions, here are the types of medications that have most commonly been cited in recent alerts:
- Hormonal Contraceptives: Especially certain types of “third-generation” birth control pills.
- Some Anti-Inflammatory Drugs: (e.g., certain NSAIDs, particularly with long-term use or high doses).
- Certain Diet Pills or Appetite Suppressants: Due to their impact on the cardiovascular system.
- Specific formulations of COVID-19-related therapies and vaccines: (In very rare cases, and often with specific age or risk factor considerations).
Important: This information is general. DO NOT stop any medication without consulting your doctor. Your healthcare provider is the only one who can assess your individual risk and guide you on alternatives.
Who Needs to Be Extra Vigilant? Understanding Your Risk Factors
The risk of clot-related events from these medications seems to be more pronounced in individuals with pre-existing conditions. If you have any of the following, extra caution and discussion with your doctor are crucial:
- High blood pressure
- Smoking history
- Obesity
- Diabetes
- Genetic clotting disorders
- A personal or family history of blood clots
Urgent Red Flags: Symptoms You MUST Watch Out For
Time is absolutely critical when it comes to blood clots. If you are taking any medication and experience any of the following symptoms, seek immediate medical attention (call emergency services or go to the nearest ER):
- Sudden Chest Pain: Especially if it feels sharp or worsens with breathing.
- Shortness of Breath: Sudden difficulty breathing, or feeling like you can’t get enough air.
- Unexplained Swelling in the Legs or Arms: Often accompanied by pain, redness, or warmth.
- Severe Headache or Visual Disturbances: Especially if sudden and unlike typical headaches.
- Rapid Heartbeat or Irregular Pulse: A sudden change in your heart’s rhythm.
- Sudden Weakness or Numbness: Especially on one side of the body, or difficulty speaking.
Even if you’re unsure, it’s always better to be evaluated by a doctor than to ignore potential warning signs.
Your Action Plan: What to Do If You’re Concerned
- DO NOT Stop Your Medication Abruptly: This is crucial. Stopping certain medications without medical guidance can cause more harm than continuing them.
- Contact Your Doctor IMMEDIATELY: Schedule an urgent appointment or call your healthcare provider. Discuss your concerns, your medications, and your personal risk factors. Ask about alternative treatments or a personalized risk assessment.
- Stay Informed: Rely on trusted, official sources like your national health authority (e.g., FDA, EMA, CDC) or your local health department. Avoid unverified information on social media.
- Report Side Effects: If you experience any adverse reactions, report them to your national health authority’s adverse event reporting system. Your report contributes to public safety data and helps identify emerging risks.
Your awareness and proactive communication with your healthcare team are your strongest defenses. Stay vigilant, stay informed, and prioritize your health.
Have you or someone you know experienced unexpected side effects from medication? Share your story (anonymously if preferred) to help others stay informed. Let’s create a community of vigilance!